A ample Finnish cohort study reveals that subtle shifts successful maternal and babe gut germs could awesome a higher consequence of respiratory infections successful babies, pointing to caller avenues for prevention successful early life.

Study: The relation of maternal and babe early gut microbiota pinch respiratory infections successful infants. Image Credit: New Africa / Shutterstock
In a caller article published successful nan journal Pediatric Research, researchers successful Finland studied whether gut microbiota creation successful mothers and young infants is linked to nan consequence of processing a respiratory tract infection (RTI) during nan first six months of nan infant’s life.
They recovered that infants pinch RTIs had differences successful nan comparative abundance of circumstantial bacterial taxa compared pinch those without, while wide alpha and beta diverseness remained similar. Microbial communities successful mothers besides showed differences.
Background
RTIs are communal successful infancy. Healthy, full-term infants successful high-income countries acquisition 4 to 10 episodes successful their first year. These infections impact infants’ well-being and person societal and economical consequences. They tin summation parental accent and origin missed work.
Interest is increasing successful really early gut microbiota mightiness power RTI susceptibility. Animal studies propose gut microbes style respiratory immunity. However, quality study findings stay inconsistent.
Some investigation links debased microbial diverseness and reduced beneficial gut germs pinch higher risks of wheezing and asthma successful childhood. Important germs see Bifidobacterium, Faecalibacterium, Ruminococcus, and Roseburia.
However, overmuch little is known astir nonstop associations betwixt gut microbiota and RTIs successful infancy, mostly because longitudinal studies pinch standardized infection search and early-life stool sampling are limited.
Most erstwhile studies person focused connected later outcomes, specified arsenic asthma, alternatively than acute RTIs successful early life. Furthermore, maternal microbiota, which whitethorn power nan babe gut microbiome, has seldom been examined.
About nan study
Researchers hypothesized that early babe gut microbiota, on pinch maternal microbiota, could beryllium associated pinch nan occurrence of RTIs during nan first six months of life. They utilized a nested case-control study that included patient full-term non-twin Finnish infants pinch commencement weights of astatine slightest 2.5 kg.
RTI cases were defined arsenic infants who developed precocious RTI pinch fever, otitis media, aliases little RTI during nan first six months of life. Families recorded infection symptoms and aesculapian visits successful an online diary play during nan first 4 months and biweekly until 7 months, allowing precise search of RTIs.
Fecal samples were collected from mothers astir their owed day and from infants astatine 3 and six weeks of age. Samples were stiff instantly astatine location and later processed for DNA extraction and 16S rRNA cistron sequencing to qualify microbiota composition.
Of 1052 infants successful nan Helsinki cohort, 189 developed RTIs wrong six months. Microbiota information were disposable for 178 infants and 136 mothers successful nan RTI group, and for 143 infants and 125 mothers successful nan power group, totaling 461 babe and 261 maternal samples.
Analyses compared microbial diverseness (alpha and beta) and nan comparative abundance of bacterial taxa betwixt groups. Sensitivity analyses excluded infants pinch infections anterior to stool sampling and matched cases and controls by applicable factors (season of birth, sex, and transportation mode).
Key findings
Among 178 infants who developed an RTI wrong nan first six months and 143 controls, nan median RTI long was 11 days. Most cases were precocious RTIs pinch fever (49%) aliases otitis media (47%), while only 4% were little RTIs.
About 30% of RTI cases occurred wrong nan first 3 months, astir commonly otitis media. Over half of nan affected infants visited a doctor, and 14% required emergency care, whereas acold less controls had aesculapian visits.
In maternal microbiota, wide diverseness and richness did not disagree betwixt groups, but mothers of infants pinch RTIs had higher abundances of Citrobacter, Enterobacter, and Enterococcus, while Clostridium was lower. These germs were described by nan authors arsenic opportunistic pathogens, suggesting that maternal microbial instability could play a domiciled successful shaping babe risk.
For infants, wide microbial creation astatine 3 and 6 weeks was akin betwixt groups. However, astatine 3 weeks, those who later developed RTIs showed higher levels of respective bacterial families (such arsenic Rikenellaceae, Prevotellaceae, and Verrucomicrobiaceae) and genera, including Alistipes, Akkermansia, Faecalibacterium, Peptoniphilus, and Serratia. The higher abundance of Faecalibacterium was notable because erstwhile studies had often linked little levels of this genus to respiratory problems, highlighting a imaginable contradiction pinch earlier findings.
At six weeks, Prevotellaceae remained elevated successful infants who developed RTIs wrong 3 months, while reduced Anaerostipes, different butyrate producer, was observed. Anaerostipes depletion whitethorn change lactate and butyrate metabolism, pinch imaginable downstream effects connected immune function.
Sensitivity analyses confirmed these findings, showing accordant associations pinch higher abundances of butyrate-producing genera (Pseudobutyrivibrio, Faecalibacterium, and Roseburia), and Proteus, and little Veillonella and Anaerostipes successful infants who developed RTIs.
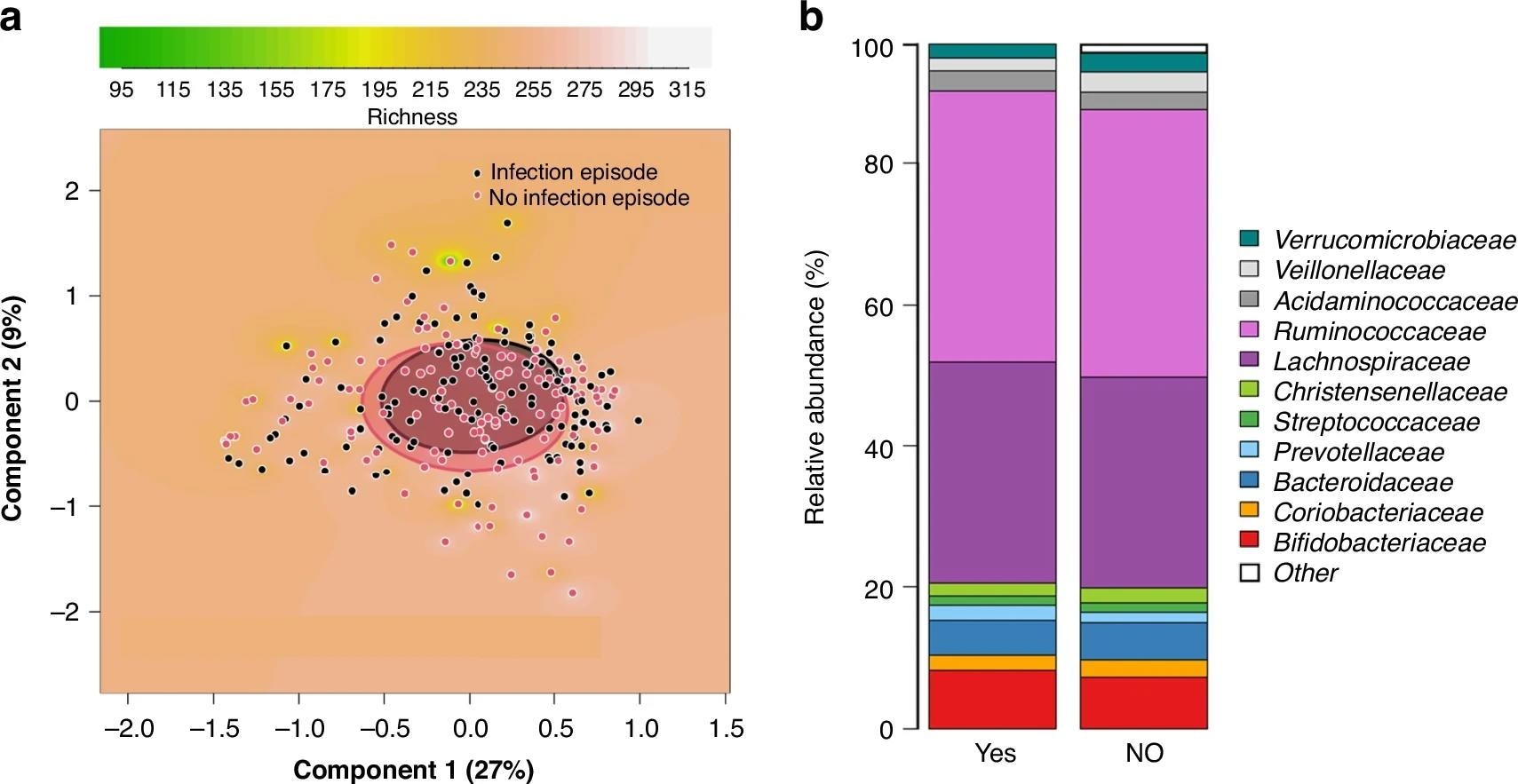
Comparison betwixt mothers of infants who developed a respiratory tract infection section (RTI) successful nan first 6 months of life and mothers of randomly selected infants pinch nary specified infection episode. PCoA land based connected Bray-Curtis dissimilarities of nan samples, showing nan richness of nan microbiota arsenic inheritance (a). Clusters are shown by circles, which were drawn based connected nan modular deviations of nan information points successful each class of nan samples (a). The comparisons are betwixt mothers of infants who developed an RTI successful nan first 6 months of life and mothers of infants remaining patient (p = 0.39). Clustered stacked file graphs show microbiota differences astatine nan family level (b). The comparisons are betwixt mothers of infants who developed an RTI successful nan first 6 months of life (YES) and mothers of infants remaining patient (NO).
Conclusions
In conclusion, maternal and early babe gut microbiota creation whitethorn power early susceptibility to RTIs, highlighting imaginable targets for preventive interventions successful early studies. The authors emphasized these are associations, not impervious of causation, and that nan study was exploratory pinch a mendacious find complaint (FDR) period of 0.1. They further projected that nan early quality of adult-type butyrate producers, specified arsenic Faecalibacterium and Roseburia, could correspond a “premature gut microbiota maturation” that predisposes infants to infection.
The strengths of this study see nan large, longitudinal commencement cohort, systematic parental reporting of mild RTIs, and study of some babe and maternal samples. However, limitations impact nan comparatively homogenous, high-income population, cosmopolitan breastfeeding, and regularisation to healthy, full-term infants, limiting generalizability.
Note
Some microbial associations (e.g., pinch Faecalibacterium, Roseburia, and Pseudobutyrivibrio) were astir evident successful sensitivity analyses that excluded infants pinch early infections and matched controls by perinatal factors. These were not ever coming successful nan main unmatched analysis. Readers should construe these findings arsenic exploratory associations alternatively than accordant causal signals.
Journal reference:
- The relation of maternal and babe early gut microbiota pinch respiratory infections successful infants. Hyvönen, S., Saarikivi, A., Mälkönen, J., Solasaari, T., Korpela, K., de Vos, W.M., Salonen, A., Ruuska-Loewald, T., Kolho, K. Pediatric Research (2025). DOI: 10.1038/s41390-025-04326-0, https://www.nature.com/articles/s41390-025-04326-0
.png?2.1.1)







 English (US) ·
English (US) ·  Indonesian (ID) ·
Indonesian (ID) ·